Nuffield Health Exeter Hospital
Wonford Rd, Exeter EX2 4UG
Tel: 01392 262 122

Arthritis
Jump to:
What is arthritis?
"Put simply, arthritis occurs when a joint loses its smooth cartilage which results in friction and leads to inflammation and pain".
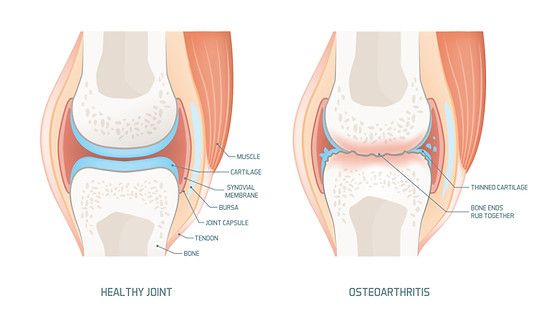
Cartilage is a smooth white substance that covers the ends of the bones in our joints. It acts as a shock absorber and allows for smooth movement of the joint.
There are many reasons why we may lose this cartilage and the underlying bone can eventually become exposed.
Rather than smooth cartilage gliding on smooth cartilage, sensitive bone ends then rub together causing inflammation and pain.
What causes arthritis?
Arthritis is extremely common and an inevitable part of the ageing process. There are many different causes but in the majority of cases, the treatment is the same.
Common Causes of arthritis:
-
Advancing age (leading to wear and tear of the joints). This often has a slow and gradual progression.
-
Trauma. Injuries can lead to a form of arthritis which is often more advanced and occurs over a shorter period of time.
-
Infection. If this occurs within a joint it can lead to rapid destruction of the cartilage and a more severe form of arthritis.
-
Inflammation. There are several rheumatological conditions that can lead to destruction of joints. The mechanism is slightly different to those described above but can result in a severe form of arthritis. The condition rheumatoid arthritis would be an example of this.
What are the signs & symptoms of arthritis?

The most common and consistent symptom of arthritis in the hand is pain.
Joint pain. This is very subjective and personal to the individual experiencing it. It is often described as a dull ache with intermittent sharp components and is commonly compared to a toothache. The pain can remain localised to one place or it can refer up or down from the affected area.
Sleep disturbance. This is a common feature of arthritis and patients often describe difficulty in being able to get off to sleep due to pain or waking in the night as a result of it.
Loss of function. Once a joint loses its cartilage it will start to lose movement. This usually occurs over a long period of time and as a result may not be noticed until the individual loses the ability to perform a specific task.

Swelling and deformity.
Once the cartilage has started to wear down the joints can become swollen and inflamed. The body's early response to this damage is to produce an excess of lubricating fluid which leads to additional swelling, warmth, pain and restriction of movement.
Over time, greater destruction of the joints can occur due to this inflammation and mechanical wear and this in turn can lead to the formation of bony growths known as osteophytes. Once again these can lead to reduced movement and function.
Joint deformity can occur with progressive destruction leading to an abnormal angulation of the joint. This can affect function but also can be cosmetically unacceptable.
Diagnosis and Investigations
The diagnosis of arthritis is commonly made from the history and examination alone.
We use simple X-rays to confirm the type of arthritis and its location as well as severity. This helps to give a prognosis and create a management plan.
Occasionally a CT scan or MRI scan may be recommended. These scans can give extra detail and allow evaluation of the bone architecture or soft tissue structures which can also be involved. The use of these scans can be helpful for pre-operative planning.
Whilst simple X-rays will normally be available to you at your initial visit, CT or MRI scans will need to be booked at a second visit at a time convenient to you.
Treatment
The treatment of arthritis usually starts with non surgical measures. Surgery is only recommended once all of these options have been exhausted and the symptoms are persisting and affecting ones quality of life.
Observation
The majority of us will develop arthritis at some point during our lives. It is important to realise that it is a normal part of the ageing process and we cannot prevent our joints from wearing out. For many patients, being given the correct diagnosis and reassurance is enough to give them peace of mind. For some however, the severity of the pain, loss of function or deformity is more problematic. These patients may be recommended to have further treatment as once severe deformity has occurred, it can be difficult to salvage later.
Hand Therapy
Hand therapists are highly specialised professionals that come from an occupational therapy or physiotherapy background. Due to the complexity of hand function their skills are essential in the treatment and postoperative management of hand conditions.
-
Education. Once we understand a condition we are in a better position to manage it. Your hand therapist will give you support and advice on how best to help manage your pain.
-
Splinting. Our hand therapists can provide you with splints to reduce movement in the arthritic joint, which will help improve your pain. Some are standard splints which come in a variety of sizes while others will be custom made for you and your condition.
-
Rehabilitation. Often pain can be improved by strengthening the muscles around the affected joints and movement can be maintained with exercises designed to not overload them. Following surgery, hand therapy is vital to regain function and improve outcomes.
-
Scar and pain management. Some patients suffer with chronic pain and hand therapists are trained to identify and treat this. Scars relating to trauma or surgery can cause problems such as sensitivity. Hand therapists can help treat this problem and encourage scars to heal in a healthy way.
Splints
Splints are medical devices that differ in shape,size and material. Some are extremely simple while others are complex and are customised for the individual.
The basic function of splints is to;
-
Prevent movement - the splint is designed to stop all movement in a specific joint. This is used for conditions such as arthritis where the pain is due to an abnormal and worn joint.
-
Prevent abnormal movement - the splint is designed to allow movement in the normal directions but to prevent abnormal movements. This is used to support damaged ligaments or to prevent deformity in joints.
-
Allow function - despite the aim of preventing or restricting movement the splint must allow useful function in the hand otherwise they will not be tolerated by the user and discarded.
-
Comfort - they must be comfortable to encourage long term use and enable the benefits to be achieved.
Examples of types of splints commonly used

Arthritis of the finger
This is a customised splint made from a plastic material with velcro straps. It has been designed to stop movement of the finger and help with pain. It is lightweight, durable and can be removed and washed.

Arthritis of the thumb
This splint is removable, lightweight and breathable. It is manufactured in a variety of sizes to fit most individuals. Often there will be a solid metal strut contained within the splint to add strength. The fingers are left free to maintain movement and function.

Arthritis of the wrist
Similar to the splint above, this splint will restrict wrist movement and is used to treat pain from wrist arthritis. Once again it is removable, lightweight and breathable and houses a metal strut to support the wrist. The thumb and fingers are free to move and allow good function.
Steroid injections
Steroids belong a family of anti-inflammatory medications and can be injected directly into joints. A steroid injection may reduce existing inflammation and therefore improve symptoms.
They are generally safe and have few side effects and can be safely used during pregnancy and breastfeeding. The improvement may take a few weeks to occur. Injections will not cure the underlying problem but can enable significant pain relief for some time. The length of the benefit is variable but can last around 6 months. A small percentage do not gain significant improvement.
Joint injections may be offered at your initial consultation and performed in the clinic rooms. In some circumstances the joint may be deep, or difficult to access and in these circumstances you may be offered the injection with the aid of ultrasound or X-ray.
There are some specific risks to be aware of.
-
Loss of pigment. The steroid can cause a loss of normal skin pigment (change in skin colour) at the injection site which may be temporary or permanent.
-
Fat atrophy. The injection can lead to some loss of fat under the skin which may alter the skin's contour.
-
Infection. There is a very small risk (around 1%) of introducing infection into the soft tissues or the joints. This might lead to pain, redness and swelling around the injection site. Mild infections may need antibiotics but more severe infections which are very rare may need admission to hospital for treatment.
-
Nerve injury. There is an extremely small risk of injury to the superficial nerves. If the needle or steroid is injected directly into the nerve in error rather than into the joint space it could cause temporary or permanent damage leading to a loss of sensation and/ or function.
-
Erratic diabetic control. As with any other steroid medication some patients with diabetes, particularly those on insulin, may find that their blood sugar levels fluctuate following the steroid injection. Close blood sugar monitoring is therefore advised following the procedure.
-
Flare up of symptoms. One in ten individuals may experience an increase in their pain following the injection which can be severe and last for a few days. Rest and painkillers are often sufficient to manage this.
Specific types of arthritis affecting the hand and wrist



Distal interphalangeal joint arthritis (DIPJ)
These joints are at the end of the finger and are a commonly affected by arthritis. Patients often complain of painful nodules over the area coupled with stiffness and difficulty in gripping objects.
Hand therapy, splinting and injections are the first treatments to consider. If these fail then the most common and successful surgical option is to fuse the joint.
Joint replacements, whilst an option, are not as successful as joint fusions and are only recommended in rare circumstances.
Proximal interphalangeal joint arthritis (PIPJ)
These joints have a large range of movement and are very important for hand function. There is an extremely delicate balance of tendons that allow these joints to work and any problems with these structures lead to stiffness and a significant loss of grip. Loss of movement in these joints have the most significant impact on hand function compared to other joints.
If non- surgical management fails, surgery is recommended in the form of either a joint fusion or replacement.
Metacarpal
phalangeal joint arthritis (MCPJ)
These are the joints that connect the fingers to the hand and are affected less commonly by arthritis than the two areas mentioned above.
If non- surgical management fails surgery is recommended.
Joint fusions are not a great option here as mobility in these joints is essential for grip. Joint replacement is the standard operation offered.

Distal radioulnar joint arthritis (DRUJ)
The DRUJ is the joint that allows pronation and supination of the wrist (turning the palm to face up and face down). Arthritis of this joint is rare but can lead to pain on these movements.
If conservative measures fail, surgery may be considered.
There are many surgical options, and the most suitable procedure for you will depend on several different factors, which include; your age, functional status and the underlying cause of your symptoms.
Joint resection
In basic terms the end of the ulna bone (one of the bones of your wrist) can be removed. This procedure can improve pain and is effective, particularly for patients who have low physical demand.
Joint replacement
Another option is to perform a joint replacement.
The joint can be replaced with half a new joint, or a total joint. In general these tend to give better functional outcomes when compared to the previous option, but is a bigger operation with greater risks.
Once you have had a chance to meet with your surgeon, the risks and benefits of these procedures will be discussed in detail and you will then be able to make an informed decision on how to proceed.

Wrist arthritis
The wrist joint is a complicated joint that consists of 10 bones that allow movement in a variety of directions.
Wrist arthritis can occur due to simple wear and tear but is often secondary to trauma such as a broken wrist or ligament injury.
Arthritis affecting the wrist is luckily not that common but can cause significant pain and loss of function if it occurs.
If non- surgical management fails then surgery can be considered.
Surgical options for wrist arthritis include;
1. Wrist denervation
This procedure is considered minor surgery and involves the selective removal of nerves that supply the joint with pain sensation. We can remove these nerves and therefore improve pain. The recovery is quick and the risks are minimal.
2. Limited fusion procedures
As there are many joints involved in wrist movement we are sometimes able to perform surgery where the bad (arthritic) parts of the wrist are fused together. The unaffected parts are left alone. These procedure are successful at improving pain and maintaining some movement.
3. Total wrist fusion
When a wrist is too severely affected with arthritis limited fusion procedures may not be an option. In this situation a total wrist fusion or wrist replacement would be recommended.
In a total wrist fusion any remaining cartilage is removed and the underlying bones are left exposed. This tricks the body into attempting to heal the bones in the same way that occurs with a fractured or broken bone. Usually the wrist joint is held together with a metal plate and screws whilst healing occurs. It takes between 6 and 8 weeks for the the wrist joint to become fully fused.
Once fused there will be no movement in the wrist and pain relief is usually excellent. Further surgery is not usually required. The main disadvantage is the loss of movement,
4. Total wrist replacement
Wrist replacement technology has improved significantly over the last two decades.
In the past this procedure was reserved for patients of low physical demand and in particular, patients suffering from rheumatoid arthritis.

This was due to the poor longevity of the artificial replacement or prosthesis. Over time the prosthesis loosened or wore out resulting in pain and eventually failure.
Modern day 4th generation wrist replacements have demonstrated significantly better results over their predecessors.
The longevity of the implants are now much better and last at least ten years in 86% of cases. These results now make this procedure a viable option for many more individuals.
The main advantage of wrist replacements is to give excellent pain relief and to preserve movement. The main disadvantage is that it may eventually wear out and fail and as a result may need to be revised or converted to a fusion.

aboutus
Devon Hand Surgery aims to give you an early diagnosis, rapid treatment (which can often be non-surgical) and perform any necessary surgery when required. We will also supervise your rehabilitation to ensure you have the best chance of restoring function, getting back to work and improving your quality of life.